Pericardial Effusion (PE) in Dogs (NAVLE Notes)
Pericardial effusion (PE) involves fluid accumulation in the pericardial sac, leading to cardiac tamponade and compromised heart function.
Classic Case
- Signs:
- Acute onset of weakness or collapse.
- Exercise intolerance, abdominal distention.
- Muffled heart sounds, tachycardia.
- Weak femoral pulses, jugular pulses.
- Pulsus paradoxus: Decreased pulse strength during inspiration.
- Pale mucous membranes.
Diagnosis
- Etiology:
- Cardiac Tumors: German Shepherd, Golden Retriever, Boxer, Labrador Retriever, Bulldog, Boston Terrier.
- Idiopathic PE: Golden Retriever, Labrador Retriever.
- ECG:
- Tachycardia and Low R-wave amplitude.
- Electrical Alternans: Alternating R-wave height due to the heart’s swinging motion within the fluid-filled pericardial sac (seen in 50% of cases).
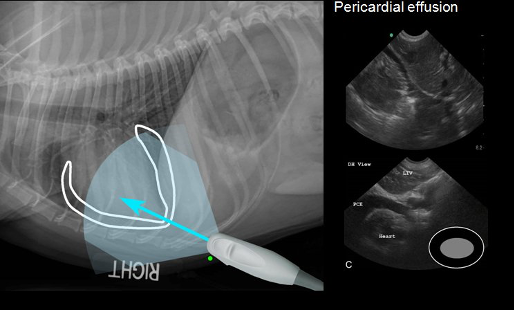
- Radiography:
- Rounded, globoid cardiac silhouette.
- Dilated caudal vena cava and ascites.
- Echocardiography:
- Confirms a fluid-filled sac surrounding the heart.
- Signs of cardiac tamponade (right heart compression).
- Possibly detects causative mass in right atrium, right auricle, or heart base.
- Cytology of Effusion:
- Limited diagnostic value except in cases of lymphoma or infection.
- Effusion PCV < 10% may improve diagnostic yield.

Treatment
- Pericardiocentesis (ultrasound-guided):
- Performed between the 4th and 6th ribs at the right costochondral junction.
- ECG monitoring during the procedure to detect arrhythmias if the heart is accidentally contacted.
- Pericardectomy:
- For recurrent effusions to reduce tamponade risk.
- Can be curative in idiopathic cases.
- Treatment of Neoplasia:
- Right Auricular Hemangiosarcoma: Possible surgical resection.
- Lymphoma, Chemodectoma, Hemangiosarcoma, Mesothelioma: Chemotherapy options available.
Key Points
- Prognosis:
- Idiopathic PE: Generally favorable if effusions are infrequent or managed with pericardectomy.
- Neoplastic PE: Poor prognosis, especially with recurrent effusions or metastatic disease.
- Chemodectoma: Guarded prognosis; pericardectomy may extend survival.
- Ultrasonography:
- Diagnostic for PE and aids in identifying underlying causes, such as tumors.
- Feline PE:
- Often linked to heart failure, unlike in dogs.
NAVLE-Style Practice Questions on Pericardial Effusion
Question 1
A 7-year-old Boxer is presented with exercise intolerance, abdominal distension, muffled heart sounds, and weak femoral pulses. ECG reveals electrical alternans. What is the most likely diagnosis?
- A) Dilated cardiomyopathy
- B) Pericardial effusion
- C) Aortic stenosis
- D) Mitral valve disease
Correct Answer: B
Explanation: The presence of exercise intolerance, abdominal distension, muffled heart sounds, weak pulses, and ECG findings of electrical alternans strongly suggests pericardial effusion.
Question 2
An ultrasound-guided pericardiocentesis is performed on a dog with recurrent pericardial effusion. During the procedure, what is a critical aspect of monitoring?
- A) Serum electrolytes
- B) Oxygen saturation
- C) ECG to detect arrhythmias
- D) Blood pressure
Correct Answer: C
Explanation: ECG monitoring is essential during pericardiocentesis to identify arrhythmias that may occur if the needle contacts the heart.
Question 3
A Golden Retriever presents with signs of pericardial effusion. Echocardiography shows a mass on the right atrium. What is the likely prognosis?
- A) Good, with curative potential using antibiotics
- B) Poor, due to neoplastic origin
- C) Guarded, with prolonged survival possible with NSAIDs
- D) Good, with supportive care only
Correct Answer: B
Explanation: A mass on the right atrium in a dog with pericardial effusion often indicates a neoplastic origin, such as hemangiosarcoma, which has a poor prognosis.
For study notes visit cracknavle.com