Overview
Remember the Types and Key Clinical Signs
- Tetanus (C. tetani): Muscle rigidity, stiff gait, third eyelid prolapse, history of metritis or wound
- Black Disease (Clostridium novyi type B): Icterus; associated with liver damage (e.g., flukes)
- Blackleg (C. chauvoei): Acute lameness, swollen muscles, crepitus, fever, often fatal
- Bacillary Hemoglobinuria (C. haemolyticum): Icterus, hemoglobinuria (“red water”), liver fluke association
- Gas Gangrene (C. perfringens and others): Malodorous, crepitant wounds; rapid necrosis
- Enterotoxemia (C. perfringens type D): Sudden death, bloat, colic in young animals
- Malignant Edema (C. septicum): Necrotizing fasciitis, wound infections, swelling
- Hemorrhagic Bowel Syndrome (C. perfringens type A, β-2 toxin): High-producing dairy cow with colic, “blackberry jam” feces
- Botulism (C. botulinum): Flaccid paralysis—weak tongue, tail, eyelids, jaw, anus; recumbency
Lets see a typical NAVLE Styled Question
A 4-year-old multiparous Holstein cow in peak lactation is found lying in her stall, reluctant to rise, with mild abdominal distention and signs of colic. She is dull, tachycardic (HR 112 bpm), and her mucous membranes are injected. Rectal exam reveals decreased fecal output, and her manure appears dark, gelatinous, and blood-tinged—described by the owner as “blackberry jam.” The cow was reportedly normal the previous day, and no other animals in the herd are currently affected.
The farm recently had issues with moldy silage and has a high-producing herd under intensive management. The cow has been vaccinated with a 7-way clostridial vaccine but not within the past year. No evidence of external wounds is found.
Which of the following is the most likely diagnosis, and what is the best next step?
A. Clostridium tetani infection; administer tetanus antitoxin and systemic penicillin
B. Hemorrhagic bowel syndrome; initiate aggressive IV fluid therapy and consider surgical correction
C. Enterotoxemia due to C. perfringens type D; administer clostridial antitoxin and oral antibiotics
D. Bacillary hemoglobinuria; test for liver flukes and treat with flukicide and antimicrobials
E. Botulism; give polyvalent botulinum antitoxin and supportive care
Correct Answer: B. Hemorrhagic bowel syndrome; initiate aggressive IV fluid therapy and consider surgical correction
Explanation:
This is a classic case of Hemorrhagic Bowel Syndrome (HBS), also known as Jejunal Hemorrhagic Syndrome, which typically affects multiparous, high-producing dairy cows in early to peak lactation. Key features include:
- Sudden onset of colic, depression, and anorexia
- Decreased fecal output or passage of “blackberry jam”-like feces
- Often linked to Clostridium perfringens type A producing β-2 toxin
- Risk factors include high-energy diets, moldy feed, and intensive production systems
Diagnosis is usually clinical but may be supported post-mortem by finding a segment of jejunum distended with clotted blood.
Treatment is difficult and includes:
- Aggressive IV fluids to manage shock
- Exploratory surgery to manually break up or remove clotted segments
- Systemic antimicrobials and NSAIDs
- Prognosis is guarded to poor but early aggressive therapy may save the animal
Why the Other Options Are Incorrect:
- A. Tetanus: Presents with hyperesthesia, stiffness, third eyelid prolapse, and sawhorse stance, not colic or jelly-like feces
- C. Enterotoxemia (C. perfringens type D): Primarily affects young, fast-growing lambs and calves, not adult dairy cows
- D. Bacillary hemoglobinuria (C. haemolyticum): Associated with hemoglobinuria and liver fluke infestation, not colic or blood clots in the stool
- E. Botulism: Causes progressive flaccid paralysis (weak tail, tongue, eyelids), not colic or hemorrhagic diarrhea
Major Clostridial Diseases in Cattle
- Blackleg (Clostridium chauvoei)
- Etiology: Ingestion of spores that localize in muscle tissue; activation often follows muscle trauma.
- Clinical Signs: Sudden death, high fever, lameness, swelling in heavy muscles with crepitus (gas under the skin).
- Diagnosis: Post-mortem findings of dark, dry, spongy muscle tissue with a rancid odor.
- Prevention: Vaccination with multivalent clostridial vaccines.Wikipedia
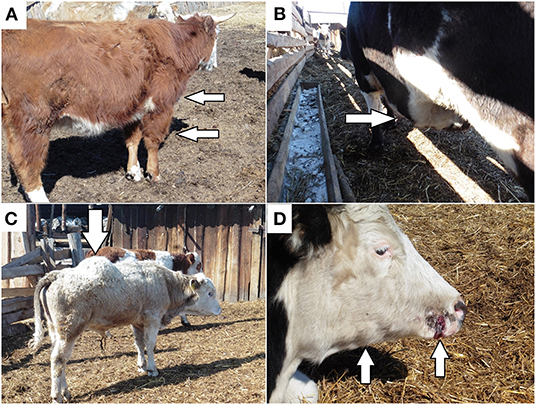
Distinct clinical signs of blackleg: (A) oedema in the scapular shoulder joint of the anterior right limb; (B) oedema in the abdominal cavity; (C) oedema in the back; (D) papilloma trauma on the cow muzzle with subsequent oedema and the formation of nodes in the subcutaneous tissue in the area of the right branch of the jaw.
- Malignant Edema (Clostridium septicum, C. sordellii, C. novyi)
- Etiology: Contamination of wounds with spores leading to local toxin production.
- Clinical Signs: Rapidly spreading swelling, edema, and gas accumulation at the wound site; high fever; depression.
- Diagnosis: Clinical signs and history of recent wounds or surgical procedures.
- Prevention: Proper wound management and vaccination.
- Black Disease (Clostridium novyi Type B)
- Etiology: Associated with liver fluke (Fasciola hepatica) migration causing liver damage, creating anaerobic conditions for spore germination.
- Clinical Signs: Sudden death; often no premonitory signs.
- Diagnosis: Necropsy revealing liver lesions and presence of flukes.
- Prevention: Control of liver flukes and vaccination.Merck Veterinary Manual
- Enterotoxemia (Clostridium perfringens Types B, C, and D)
- Etiology: Overgrowth of C. perfringens in the intestine due to sudden dietary changes, leading to toxin production.
- Clinical Signs: Sudden death, abdominal pain, diarrhea (often bloody), neurological signs in some cases.
- Diagnosis: Identification of toxins in intestinal contents; necropsy findings.
- Prevention: Gradual dietary changes and vaccination.
- Tetanus (Clostridium tetani)
- Etiology: Spore entry through wounds; toxin affects nervous system.
- Clinical Signs: Muscle stiffness, “lockjaw,” prolapse of the third eyelid, sensitivity to stimuli.
- Diagnosis: Clinical signs and history of recent wounds.
- Prevention: Vaccination and proper wound care.Cornell Vet School
- Botulism (Clostridium botulinum)
- Etiology: Ingestion of preformed toxin in contaminated feed or water.
- Clinical Signs: Progressive muscle paralysis, difficulty swallowing, recumbency, death.
- Diagnosis: Detection of toxin in serum or feed samples.
- Prevention: Proper feed storage and vaccination in endemic areas.
Diagnosis
- Clinical Evaluation: Sudden death in well-conditioned animals; specific signs depending on the disease.
- Laboratory Tests: Detection of toxins, bacterial culture, PCR assays.
- Necropsy Findings: Characteristic lesions in muscles or organs; gas accumulation; tissue necrosis.Wikipedia
Treatment
- Antibiotic Therapy: High doses of penicillin may be effective if administered early.
- Supportive Care: Fluid therapy, anti-inflammatories, wound management.
- Antitoxins: Available for certain clostridial toxins; effectiveness varies.
Note: Due to the rapid progression of clostridial diseases, treatment is often unsuccessful, emphasizing the importance of prevention.
Prevention
- Vaccination: Routine use of multivalent clostridial vaccines (e.g., 7-way or 8-way) is crucial.
- Management Practices:
- Proper wound care and hygiene during procedures like castration and dehorning.
- Avoid sudden dietary changes; introduce new feeds gradually.
- Control of liver flukes to prevent black disease.
- Safe feed storage to prevent botulism.
NAVLE-Style Multiple-Choice Questions
Question 1:
A 12-month-old steer is found dead without prior signs. Necropsy reveals dark, dry, spongy muscle tissue with a rancid odor and gas bubbles. What is the most likely diagnosis?
A. Malignant edema
B. Blackleg
C. Enterotoxemia
D. Botulism
E. Tetanus
Correct Answer: B. Blackleg
Explanation: Blackleg, caused by Clostridium chauvoei, typically affects well-conditioned young cattle and leads to sudden death with characteristic muscle lesions.
Question 2:
Which clostridial disease is most commonly associated with liver fluke infestation in cattle?
A. Tetanus
B. Botulism
C. Black disease
D. Malignant edema
E. Enterotoxemia
Correct Answer: C. Black disease
Explanation: Black disease, caused by Clostridium novyi Type B, is often linked to liver damage from migrating liver flukes, creating anaerobic conditions conducive to spore germination.
Question 3:
What is the most effective strategy to prevent clostridial diseases in cattle herds?
A. Routine antibiotic administration
B. Regular deworming
C. Multivalent vaccination programs
D. Isolation of new animals
E. Frequent hoof trimming
Correct Answer: C. Multivalent vaccination programs
Explanation: Vaccination with multivalent clostridial vaccines is the cornerstone of prevention, providing protection against multiple clostridial pathogens.
References
- Merck Veterinary Manual: Overview of Clostridial Diseases in Animals
- NADIS: Clostridial Disease in Cattle
- Alltech: Treating and Preventing Clostridium in Cattle
- MSD Animal Health: Clostridial DiseaseMerck Veterinary Manual, nadis.org.uk and Alltech
- https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2022.872386/full