Liver Abscesses in Cattle: A Comprehensive NAVLE Study Guide
Overview
Liver abscesses (MVM) are localized bacterial infections in the liver tissue, commonly seen in feedlot cattle. They significantly impact productivity and carcass quality, often going undetected until slaughter. Subclinical cases may reduce feed efficiency, weight gain, and cause carcass trimming, while clinical cases can affect animal welfare and milk yield.

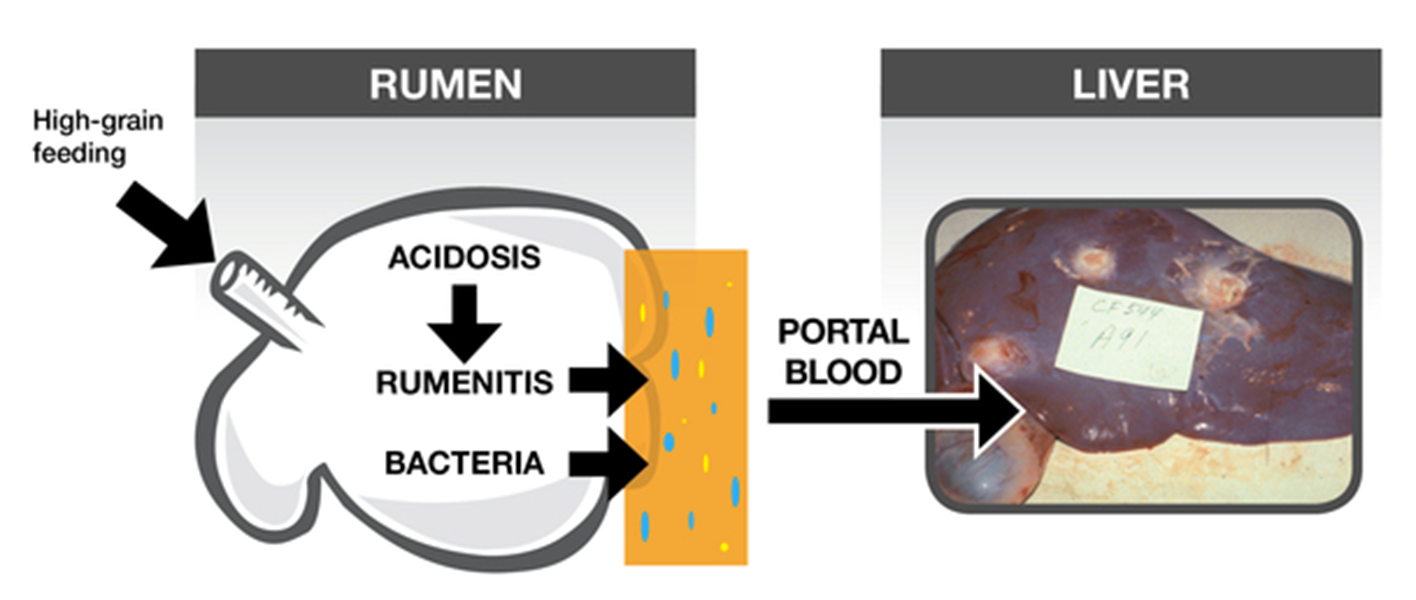
Etiology and Pathogenesis
The primary pathogen is Fusobacterium necrophorum, an anaerobic, gram-negative rod found in the rumen. High-concentrate diets cause ruminal acidosis and rumenitis, allowing bacteria to translocate into the portal circulation. Secondary invaders like Trueperella pyogenes or Streptococcus spp. may also contribute.
Bacteria lodge in the liver, particularly the right lobe, where abscesses form, sometimes coalescing into large necrotic areas. These may rupture or lead to thromboembolic pneumonia.
Epidemiology
- Affects up to 32% of feedlot cattle at slaughter
- Most common in high-concentrate, low-roughage diets
- Increased risk in Holstein steers and those with poor bunk management
- Rare in pasture-based systems
Clinical Signs
- Typically subclinical
- Decreased feed efficiency and daily gain
- Decreased milk production in dairy cattle
- Occasional signs: anorexia, fever, reluctance to move, right cranial abdominal pain
- Sudden death if abscess ruptures into the caudal vena cava (leading to hemoptysis)
Diagnosis
Ante-mortem diagnosis is difficult and rarely pursued except in valuable dairy cattle.
- Suspect in cattle with poor performance and ruminal acidosis history
- Liver enzyme elevations (GGT, AST) possible but nonspecific
- Ultrasound or exploratory laparotomy may help confirm in rare cases
Post-mortem:
- Abscesses often range from 1–10 cm
- Multiple abscesses with thick fibrous capsules
- Hepatic tissue may show chronic inflammation and necrosis
Treatment
- Rarely attempted in feedlot animals due to cost
- In dairy cattle: procaine penicillin G or ceftiofur (off-label use requires VCPR and withdrawal monitoring)
- Prognosis is guarded once clinical signs appear
Prevention and Control
Dietary management:
- Gradual adaptation to high-concentrate rations
- Include adequate fiber to minimize subacute ruminal acidosis
- Maintain consistent feeding schedules
Feed Additives:
- Tylosin phosphate: 60–90 mg/head/day, significantly reduces incidence
- Virginiamycin is an alternative, especially in combination with tylosin
- Must be used under Veterinary Feed Directive (VFD)
Experimental vaccination: Some studies on F. necrophorum toxoid vaccines show potential, but no licensed product is available in North America.
NAVLE-Style Multiple-Choice Questions
Question 1:
A 16-month-old feedlot steer on a high-concentrate diet shows no clinical signs but is found at slaughter to have multiple encapsulated liver lesions. What is the most likely cause?
A. Salmonella dublin
B. Trueperella pyogenes
C. Fusobacterium necrophorum
D. Clostridium novyi
E. Pasteurella multocida
Correct Answer: C. Fusobacterium necrophorum
Explanation: This anaerobe is the primary cause of liver abscesses in cattle, particularly those fed high-grain diets that predispose to rumenitis and bacterial translocation.
Question 2:
Which of the following interventions best reduces liver abscesses in feedlot cattle?
A. Flunixin meglumine injection
B. Free-choice mineral blocks
C. Tylosin inclusion in the ration
D. Restricting water intake
E. Increased grain intake
Correct Answer: C. Tylosin inclusion in the ration
Explanation: Tylosin, administered in feed, significantly reduces the prevalence of liver abscesses in finishing cattle.
Question 3:
What is the most likely pathogenesis of liver abscesses in cattle?
A. Direct hepatic penetration from external wounds
B. Migration of helminths through the liver
C. Bacterial translocation from rumen ulcerations
D. Inhalation of liver pathogens
E. Congenital vascular defects
Correct Answer: C. Bacterial translocation from rumen ulcerations
Explanation: High-starch diets can cause ruminal acidosis, rumenitis, and bacterial translocation through portal circulation to the liver.